By Dr. Kingsley Chin
Dr. Kingsley R. Chin is a board-certified Harvard-trained Orthopedic Spine Surgeon and Professor with copious business and information technology exposure. He sees a niche opportunity where medicine, business and info. tech meet – and is uniquely educated at the intersection of these three professions. He has experience as Professor of Clinical Biomedical Sciences & Admissions Committee Member at the Charles E. Schmidt College of Medicine at Florida Atlantic University, Professor of Clinical Orthopedic Surgery at the Herbert Wertheim College of Medicine at Florida International University, Assistant Professor of Orthopaedics at the University of Pennsylvania Medical School, Visiting Spine Surgeon & Professor at the University of the West Indies, Mona, and Adjunct Professor of Clinical Biomedical Sciences at the University of Technology, Jamaica.Scientific Paper
Chin KR1, Coombs AV, Seale JA.
Interested medical professionals can read through the full paper, as published in Spine, here.
Study Design
Retrospective study.
Objective
To report surgical and patient-reported outcomes after outpatient lumbar fusions in an ambulatory setting.
Summary of Background Data
There is growing interest in the potential benefits of outpatient spine surgery such as reduced costs, consistent operative team, and decreased postoperative complications during in-hospital recovery. However, there are limited studies on outcomes after outpatient lumbar fusions, to guide patient selection, treatment techniques and postoperative expectations.
Methods
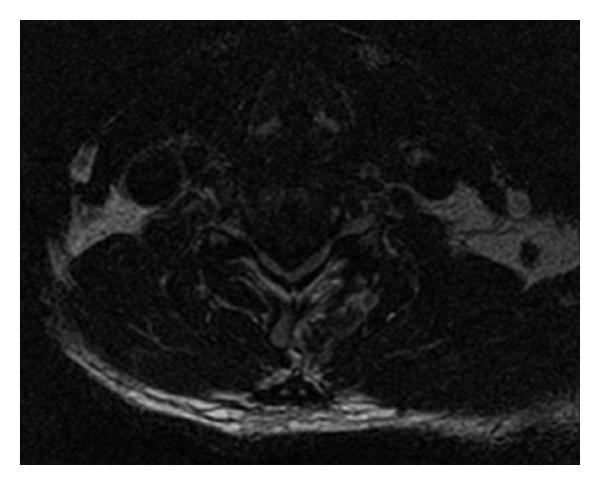
Medical records of 16 consecutive patients, who underwent outpatient direct open, single-level, posterior lumbar interbody fusions, were examined by a single surgeon. Outcome measures included visual analogue scale (VAS) scores for lower back and Oswestry Disability Indices (ODIs). Mean body mass indices (BMIs), estimated blood loss, surgical times and complications, and fusion rates were evaluated.
Results
Males represented 56% of patients. Mean age was 42.81 ± 3.05 years (mean ± standard error) and mean body mass index was 28.95 ± 1.04. History of smoking and narcotics use were statistically noncontributory. Mean final follow-up was 15 (range, 5.52-34.2 mo) months. Mean postoperative scores were determined by the final follow-up VAS and ODI. L5-S1 was the most common level of the 16 levels operated on (69%). Preoperative and postoperative VAS and ODI scores for lower back were obtained for 15 patients (93.75%). Mean lower back VAS score of 8.4 ± 0.37 preoperatively reduced to 4.96 ± 0.73 postoperatively, (P = 0.001). Mean ODI improved from 52.71 ± 0.04 preoperatively, to 37.43 ± 0.06 postoperatively, (P = 0.04). One patient experienced postoperative worsened back pain with clinical and radiological signs of possible aseptic discitis. Estimated blood loss was 161 ± 32 mL and average operating time was 124.85 ± 7.10 minutes. The overall fusion rate was 87.5%.
Conclusion
Direct open posterior lumbar interbody fusions were done safely with statistically significant reduction in average pain and ODI scores. Surgical times were approximately 2 hours with minimal blood loss, allowing patients to be comfortably discharged the same day without a drain.
About Author Dr. Kingsley R. Chin
Dr. Kingsley R. Chin, Founder of philosophy and practice of The LES Society and The LESS Institute
Dr. Kingsley R. Chin is a board-certified Harvard-trained Orthopedic Spine Surgeon and Professor with copious business and information technology exposure. He sees a niche opportunity where medicine, business and info. tech meet – and is uniquely educated at the intersection of these three professions. He has experience as Professor of Clinical Biomedical Sciences & Admissions Committee Member at the Charles E. Schmidt College of Medicine at Florida Atlantic University, Professor of Clinical Orthopedic Surgery at the Herbert Wertheim College of Medicine at Florida International University, Assistant Professor of Orthopaedics at the University of Pennsylvania Medical School, Visiting Spine Surgeon & Professor at the University of the West Indies, Mona, and Adjunct Professor of Clinical Biomedical Sciences at the University of Technology, Jamaica.
Learn more about Dr. Chin here and connect via LinkedIn.
About Less Exposure Surgery
Less Exposure Surgery (LES) is based on a new philosophy of performing surgery, leading the charge to prove through bench and clinical outcomes research that LES treatment options are the best solutions – to lowering the cost of healthcare, improving outcomes and increasing patient satisfaction. Learn more at LESSociety.org.
The LES Society philosophy: “Tailor treatment to the individual aiding in the quickest recovery and return to a pain-free lifestyle, using LES® techniques that lessen exposure, preserve unoffending anatomy and utilize new technologies which are safe, easy to adopt and reproducible. These LES®techniques lessen blood loss, surgical time and exposure to radiation and can be safely performed in an outpatient center. Less is more.” – Kingsley R. Chin, MD
About The LESS Institute
The LESS Institute is the world leader center of excellence in Less Exposure Surgery. Our safe, effective outpatient treatments help patients recover quickly, avoid expensive hospital stays and return home to their family the same day. Watch our patient stories, follow us on Facebook and visit TheLESSInstitute.com to learn more.
About SpineFrontier
The above study utilized LES Technology from SpineFrontier – leading provider of LES Technologies and instruments – offering surgeons and patients superior technology and services.
Scientific Paper Author and Citation Details
Authors
Chin KR1, Coombs AV, Seale JA.
Author information
*Department of Clinical Biomedical Sciences, Charles E. Schmidt College of Medicine at Florida Atlantic University, Boca Raton, FL †Less Exposure Surgery Specialists Institute (LESS Institute), Fort Lauderdale, FL; and ‡Less Exposure Surgery Society (LES Society), Beverly, MA.